
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- The Association between Pulmonary Functions and Incident Diabetes: Longitudinal Analysis from the Ansung Cohort in Korea (Diabetes Metab J 2020;44: 699-710)
- Hoon Sung Choi, Sung Woo Lee, Jin Taek Kim, Hong Kyu Lee
- Diabetes Metab J. 2020;44(6):944-945. Published online December 23, 2020
- DOI: https://doi.org/10.4093/dmj.2020.0249
- 3,451 View
- 61 Download
- Metabolic Risk/Epidemiology
- The Association between Pulmonary Functions and Incident Diabetes: Longitudinal Analysis from the Ansung Cohort in Korea
- Hoon Sung Choi, Sung Woo Lee, Jin Taek Kim, Hong Kyu Lee
- Diabetes Metab J. 2020;44(5):699-710. Published online April 16, 2020
- DOI: https://doi.org/10.4093/dmj.2019.0109
- 6,149 View
- 104 Download
- 9 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
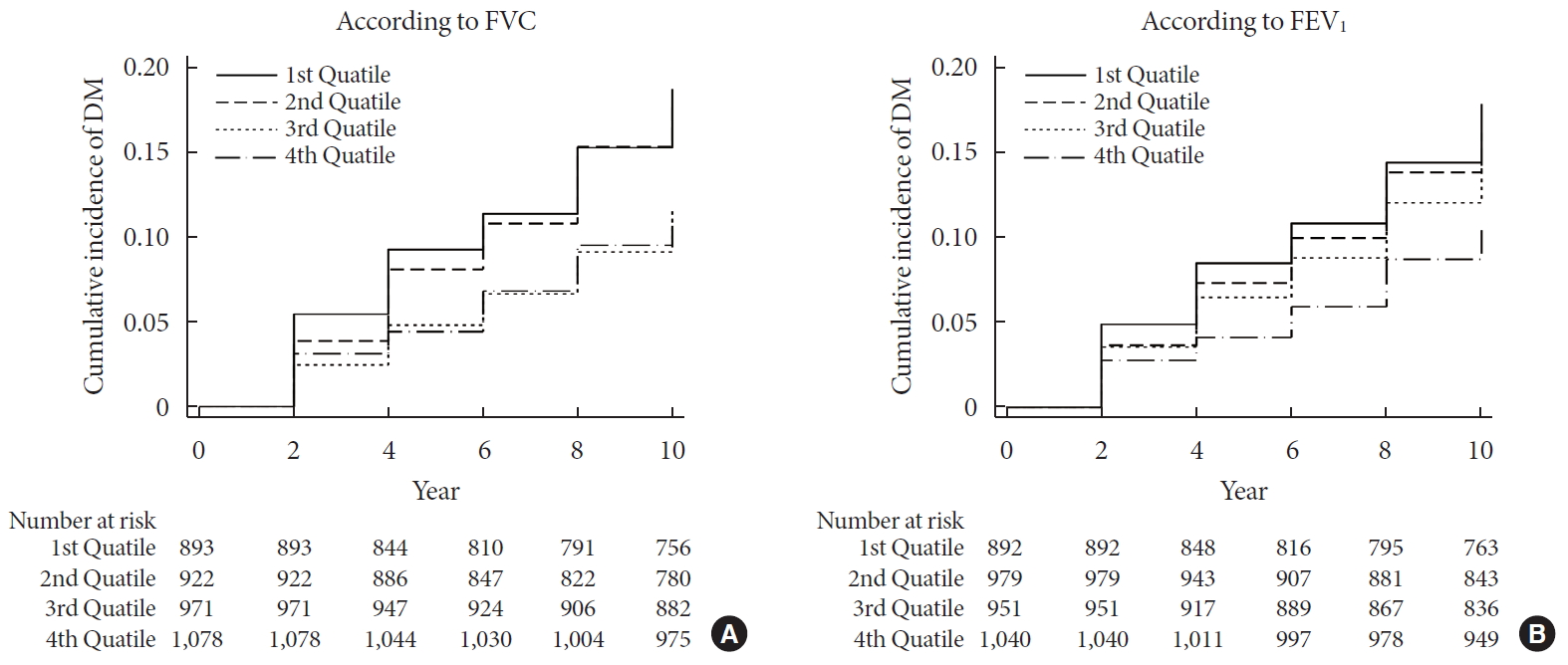
ePub Background We sought to explore whether reduced pulmonary function is an independent risk factor for incident diabetes in Koreans.
Methods We conducted a prospective cohort study of pulmonary function as a risk factor for incident diabetes using 10-year follow-up data from 3,864 middle-aged adults from the Ansung cohort study in Korea. The incidence of diabetes was assessed using both oral glucose tolerance tests and glycosylated hemoglobin levels.
Results During 37,118 person-years of follow-up, 583 participants developed diabetes (incidence rate: 15.7 per 1,000 person-years). The mean follow-up period was 8.0±3.7 years. Forced vital capacity (FVC; % predicted) and forced expiratory volume in 1 second (FEV1; % predicted) were significantly correlated with incident diabetes in a graded manner after adjustment for sex, age, smoking, exercise, and metabolic parameters. The adjusted hazard ratio (HR) and confidence interval (CI) for diabetes were 1.408 (1.106 to 1.792) and 1.469 (1.137 to 1.897) in the first quartiles of FVC and FEV1, respectively, when compared with the highest quartile. Furthermore, the FVC of the lowest first and second quartiles showed a significantly higher 10-year panel homeostasis model assessment of insulin resistance index, with differences of 0.095 (95% CI, 0.010 to 0.018;
P =0.028) and 0.127 (95% CI, 0.044 to 0.210;P =0.003), respectively, when compared to the highest quartiles.Conclusion FVC and FEV1 are independent risk factors for developing diabetes in Koreans. Pulmonary factors are possible risk factors for insulin resistance and diabetes.
-
Citations
Citations to this article as recorded by- Validation of the Framingham Diabetes Risk Model Using Community-Based KoGES Data
Hye Ah Lee, Hyesook Park, Young Sun Hong
Journal of Korean Medical Science.2024;[Epub] CrossRef - Independent and combined associations of multiple-heavy-metal exposure with lung function: a population-based study in US children
Yiting Chen, Anda Zhao, Rong Li, Wenhui Kang, Jinhong Wu, Yong Yin, Shilu Tong, Shenghui Li, Jianyu Chen
Environmental Geochemistry and Health.2023; 45(7): 5213. CrossRef - Role of Pulmonary Function in Predicting New-Onset Cardiometabolic Diseases and Cardiometabolic Multimorbidity
Guochen Li, Yanqiang Lu, Yanan Qiao, Die Hu, Chaofu Ke
Chest.2022; 162(2): 421. CrossRef - Reduced lung function predicts risk of incident type 2 diabetes: insights from a meta-analysis of prospective studies
Yunping Zhou, Fei Meng, Min Wang, Linlin Li, Pengli Yu, Yunxia Jiang
Endocrine Journal.2022; 69(3): 299. CrossRef - Development of Various Diabetes Prediction Models Using Machine Learning Techniques
Juyoung Shin, Jaewon Kim, Chanjung Lee, Joon Young Yoon, Seyeon Kim, Seungjae Song, Hun-Sung Kim
Diabetes & Metabolism Journal.2022; 46(4): 650. CrossRef - Improving Machine Learning Diabetes Prediction Models for the Utmost Clinical Effectiveness
Juyoung Shin, Joonyub Lee, Taehoon Ko, Kanghyuck Lee, Yera Choi, Hun-Sung Kim
Journal of Personalized Medicine.2022; 12(11): 1899. CrossRef - The Association between Pulmonary Functions and Incident Diabetes: Longitudinal Analysis from the Ansung Cohort in Korea (Diabetes Metab J 2020;44: 699-710)
Hoon Sung Choi, Sung Woo Lee, Jin Taek Kim, Hong Kyu Lee
Diabetes & Metabolism Journal.2020; 44(6): 944. CrossRef - The Association between Pulmonary Functions and Incident Diabetes: Longitudinal Analysis from the Ansung Cohort in Korea (Diabetes Metab J 2020;44: 699-710)
Jin Hwa Kim
Diabetes & Metabolism Journal.2020; 44(6): 940. CrossRef
- Validation of the Framingham Diabetes Risk Model Using Community-Based KoGES Data
- Plasma Glucose Regulation and Mortality in Korea: A Pooled Analysis of Three Community-Based Cohort Studies
- Nan Hee Kim, Dong-Jun Kim, Seok Won Park, Jee-Young Oh, Joong-Yeol Park, Chol Shin, Hong Kyu Lee, Yongsoo Park
- Diabetes Metab J. 2014;38(1):44-50. Published online February 19, 2014
- DOI: https://doi.org/10.4093/dmj.2014.38.1.44
- 3,815 View
- 30 Download
- 5 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Although diabetes is a well-known risk factor for death, its impact on cancer death is not clearly understood. Furthermore, it remains controversial whether impaired fasting glucose (IFG) and/or impaired glucose tolerance (IGT) are associated with increased risk of mortality. We investigated the impact of diabetes or glucose tolerance categories on all cause and cause-specific mortality.
Methods Mortality analysis was conducted in three population-based cohort studies of 3,801 participants, divided according to fasting plasma glucose (FPG) (normal; stage 1 IFG [5.6≤FPG<6.1 mmol/L]; stage 2 IFG [6.1≤FPG<7.0 mmol/L]; diabetes mellitus [DM]-FPG); or 2-hour glucose after 75 g glucose loading (2hPG) (normal; IGT; DM-2hPG), or a combination of FPG and 2hPG criteria.
Results During a median follow-up of 11.0 years, 474 subjects died from all causes. Hazard ratios (HRs) for all cause death were higher in those with diabetes as defined by either FPG or 2hPG criteria than their normal counterparts (HR, 2.2, 95% confidence interval [CI], 1.6 to 2.9 for DM-FPG; HR, 2.0, 95% CI, 1.5 to 2.7 for DM-2hPG). Similarly, diabetes defined by either FPG or 2hPG was associated with cancer death (HR, 2.9, 95% CI, 1.7 to 5.0; and HR, 2.1, 95% CI, 1.2 to 3.9, respectively). Although neither IFG nor IGT conferred higher risk for death, when combining stage 2 IFG and/or IGT, the risk of all cause death was higher than in subjects with normal glucose regulation (HR, 1.3; 95% CI, 1.0 to 1.6).
Conclusion Diabetes is associated with higher risk of death from all causes and cancer. In subjects without diabetes, stage 2 IFG and/or IGT confers increased risk for mortality.
-
Citations
Citations to this article as recorded by- Abnormal Fasting Glucose Increases Risk of Unrecognized Myocardial Infarctions in an Elderly Cohort
Richard Brandon Stacey, Janice Zgibor, Paul E. Leaverton, Douglas D. Schocken, Jennifer A. Peregoy, Mary F. Lyles, Alain G. Bertoni, Gregory L. Burke
Journal of the American Geriatrics Society.2019; 67(1): 43. CrossRef - Increased Vascular Disease Mortality Risk in Prediabetic Korean Adults Is Mainly Attributable to Ischemic Stroke
Nam Hoon Kim, Tae Yeon Kwon, Sungwook Yu, Nan Hee Kim, Kyung Mook Choi, Sei Hyun Baik, Yousung Park, Sin Gon Kim
Stroke.2017; 48(4): 840. CrossRef - β-Cell Function and Insulin Sensitivity in Normal Glucose-Tolerant Subjects Stratified by 1-Hour Plasma Glucose Values
Miranda M. Priya, Anandakumar Amutha, T.A. Pramodkumar, Harish Ranjani, Saravanan Jebarani, Kuppan Gokulakrishnan, Rajendra Pradeepa, Ranjit Unnikrishnan, Ranjit Mohan Anjana, Viswanathan Mohan
Diabetes Technology & Therapeutics.2016; 18(1): 29. CrossRef - Effect of Socio-Economic Status on the Prevalence of Diabetes
Yu Jeong Kim, Ja Young Jeon, Seung Jin Han, Hae Jin Kim, Kwan Woo Lee, Dae Jung Kim
Yonsei Medical Journal.2015; 56(3): 641. CrossRef - The Population-Based Risk of Need for Coronary Revascularization According to the Presence of Type 2 Diabetes Mellitus and History of Coronary Heart Disease in the Korean Population
Chang Hee Jung, Gi Hyeon Seo, Sunghwan Suh, Ji Cheol Bae, Mee Kyoung Kim, You-Cheol Hwang, Jae Hyeon Kim, Byung-Wan Lee, Xian Wu Cheng
PLOS ONE.2015; 10(6): e0128627. CrossRef
- Abnormal Fasting Glucose Increases Risk of Unrecognized Myocardial Infarctions in an Elderly Cohort
- Fracture Incidence and Risk of Osteoporosis in Female Type 2 Diabetic Patients in Korea
- Jong Kwan Jung, Hyo Jeong Kim, Hong Kyu Lee, Sang Soo Kim, Chan Soo Shin, Jin Taek Kim
- Diabetes Metab J. 2012;36(2):144-150. Published online April 17, 2012
- DOI: https://doi.org/10.4093/dmj.2012.36.2.144
- 4,264 View
- 38 Download
- 15 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background There are no published data regarding fracture risk in type 2 diabetic patients in Korea. In this study, we compared the fracture incidence and risk of osteoporosis of type 2 diabetic female patients with those in a non-diabetic hypertensive cohort.
Methods The incidence of fracture in a type 2 diabetic cohort was compared with that in a non-diabetic hypertensive cohort over the course of 7 years. Female type 2 diabetic and non-diabetic hypertensive patients who visited Eulji General Hospital outpatient clinic from January 2004 to April 2004 were assigned to the diabetic cohort and the non-diabetic hypertensive cohort, respectively. Surveys on fracture event, use of anti-osteoporosis medications, and bone mineral density were performed.
Results The number of fractures was 88 in the female diabetic cohort (
n =1,268, 60.6±11.5 years) and 57 in the female non-diabetic hypertensive cohort (n =1,014, 61.4±11.7 years). The RR in the diabetic cohort was 1.38 (P =0.064; 95% confidence interval [CI], 0.98 to 1.94) when adjusted for age. Diabetic patients with microvascular complications (61.0%) showed a higher RR of 1.81 (P =0.014; 95% CI, 1.13 to 2.92) compared with those without these complications. The prevalence of osteoporosis was comparable between the groups, while use of anti-osteoporosis medication was more common in the diabetic cohort (12.8%) than in the hypertensive cohort (4.5%) (P <0.001).Conclusion In our study, a higher fracture risk was observed in female type 2 diabetics with microvascular complications. Special concern for this risk group is warranted.
-
Citations
Citations to this article as recorded by- Research Progress on How to Prevent Osteoporosis in Diabetic Patients
婷玉 牛
Advances in Clinical Medicine.2022; 12(02): 1178. CrossRef - Differences in the roles of types 1 and 2 diabetes in the susceptibility to the risk of fracture: a systematic review and meta-analysis
Jiaqing Dou, Jing Wang, Qiu Zhang
Diabetology & Metabolic Syndrome.2021;[Epub] CrossRef - The risk of hip and non-vertebral fractures in type 1 and type 2 diabetes: A systematic review and meta-analysis update
Tatiane Vilaca, Marian Schini, Susan Harnan, Anthea Sutton, Edith Poku, Isabel E. Allen, Steven R. Cummings, Richard Eastell
Bone.2020; 137: 115457. CrossRef - Diabetes mellitus and risk of low-energy fracture: a meta-analysis
Jing Bai, Qian Gao, Chen Wang, Jia Dai
Aging Clinical and Experimental Research.2020; 32(11): 2173. CrossRef - Diabetes mellitus and the risk of fractures at specific sites: a meta-analysis
Hao Wang, Ying Ba, Qian Xing, Jian-Ling Du
BMJ Open.2019; 9(1): e024067. CrossRef - The use of metformin, insulin, sulphonylureas, and thiazolidinediones and the risk of fracture: Systematic review and meta‐analysis of observational studies
Khemayanto Hidayat, Xuan Du, Meng‐Jiao Wu, Bi‐Min Shi
Obesity Reviews.2019; 20(10): 1494. CrossRef - Bei Diabetikern an eine Osteoporose denken!
Stephan Scharla
MMW - Fortschritte der Medizin.2018; 160(21-22): 65. CrossRef - Type 2 diabetes and risk of low-energy fractures in postmenopausal women: meta-analysis of observational studies
Joanna Dytfeld, Michał Michalak
Aging Clinical and Experimental Research.2017; 29(2): 301. CrossRef - Risk of low-energy fracture in type 2 diabetes patients: a meta-analysis of observational studies
P. Jia, L. Bao, H. Chen, J. Yuan, W. Liu, F. Feng, J. Li, H. Tang
Osteoporosis International.2017; 28(11): 3113. CrossRef - Comorbidity and its relationship with health service use and cost in community-living older adults with diabetes: A population-based study in Ontario, Canada
Kathryn Fisher, Lauren Griffith, Andrea Gruneir, Dilzayn Panjwani, Sima Gandhi, Li (Lisa) Sheng, Amiram Gafni, Patterson Chris, Maureen Markle-Reid, Jenny Ploeg
Diabetes Research and Clinical Practice.2016; 122: 113. CrossRef - Type 2 diabetes mellitus and bone fragility: Special focus on bone imaging
Yong Jun Choi, Yoon-Sok Chung
Osteoporosis and Sarcopenia.2016; 2(1): 20. CrossRef - Epidemiology of fractures in type 2 diabetes
Ann V. Schwartz
Bone.2016; 82: 2. CrossRef - Efficacy and Safety of Weekly Alendronate Plus Vitamin D35600 IU versus Weekly Alendronate Alone in Korean Osteoporotic Women: 16-Week Randomized Trial
Kwang Joon Kim, Yong-Ki Min, Jung-Min Koh, Yoon-Sok Chung, Kyoung Min Kim, Dong-Won Byun, In Joo Kim, Mikyung Kim, Sung-Soo Kim, Kyung Wan Min, Ki Ok Han, Hyoung Moo Park, Chan Soo Shin, Sung Hee Choi, Jong Suk Park, Dong Jin Chung, Ji Oh Mok, Hong Sun Ba
Yonsei Medical Journal.2014; 55(3): 715. CrossRef - Increased Risk of Fracture and Postfracture Adverse Events in Patients With Diabetes: Two Nationwide Population-Based Retrospective Cohort Studies
Chien-Chang Liao, Chao-Shun Lin, Chun-Chuan Shih, Chun-Chieh Yeh, Yi-Cheng Chang, Yuan-Wen Lee, Ta-Liang Chen
Diabetes Care.2014; 37(8): 2246. CrossRef - Aortic Calcification and Bone Metabolism: The Relationship between Aortic Calcification, BMD, Vertebral Fracture, 25-Hydroxyvitamin D, and Osteocalcin
Kwang Joon Kim, Kyoung Min Kim, Kyeong Hye Park, Han Seok Choi, Yumie Rhee, Yong Ho Lee, Bong Soo Cha, Myong Jin Kim, Sun Min Oh, J. Keenan Brown, Sung Kil Lim
Calcified Tissue International.2012; 91(6): 370. CrossRef
- Research Progress on How to Prevent Osteoporosis in Diabetic Patients
- Prevalence and Clinical Characteristics of Recently Diagnosed Type 2 Diabetes Patients with Positive Anti-Glutamic Acid Decarboxylase Antibody
- Yul Hwangbo, Jin Taek Kim, Eun Ky Kim, Ah Reum Khang, Tae Jung Oh, Hak Chul Jang, Kyong Soo Park, Seong Yeon Kim, Hong Kyu Lee, Young Min Cho
- Diabetes Metab J. 2012;36(2):136-143. Published online April 17, 2012
- DOI: https://doi.org/10.4093/dmj.2012.36.2.136
- 4,545 View
- 40 Download
- 15 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Latent autoimmune diabetes in adults (LADA) refers to a specific type of diabetes characterized by adult onset, presence of islet auto-antibodies, insulin independence at the time of diagnosis, and rapid decline in β-cell function. The prevalence of LADA among patients with type 2 diabetes varies from 2% to 20% according to the study population. Since most studies on the prevalence of LADA performed in Korea were conducted in patients who had been tested for anti-glutamic acid decarboxylase antibody (GADAb), a selection bias could not be excluded. In this study, we examined the prevalence and clinical characteristics of LADA among adult patients recently diagnosed with type 2 diabetes.
Methods We included 462 patients who were diagnosed with type 2 diabetes within 5 years from the time this study was performed. We measured GADAb, fasting insulin level, fasting C-peptide level, fasting plasma glucose level, HbA1c, and serum lipid profiles and collected data on clinical characteristics.
Results The prevalence of LADA was 4.3% (20/462) among adult patients with newly diagnosed type 2 diabetes. Compared with the GADAb-negative patients, the GADAb-positive patients had lower fasting C-peptide levels (1.2±0.8 ng/mL vs. 2.0±1.2 ng/mL,
P =0.004). Other metabolic features were not significantly different between the two groups.Conclusion The prevalence of LADA is 4.3% among Korean adult patients with recently diagnosed type 2 diabetes. The Korean LADA patients exhibited decreased insulin secretory capacity as reflected by lower C-peptide levels.
-
Citations
Citations to this article as recorded by- The worldwide prevalence of latent autoimmune diabetes of adults among adult-onset diabetic individuals: a systematic review and meta-analysis
Deepika Ramu, Selvaraj Ramaswamy, Suresh Rao, Solomon F. D. Paul
Endocrine.2023; 82(1): 28. CrossRef - Investigation of serum level relationship anti-glutamic acid decarboxylase antibody and inflammatory cytokines (IL1-β, IL-6) with vitamins D in type 2 diabetes
Vahid Pouresmaeil, Sarmad Mashayekhi, Mohammad Sarafraz Yazdi
Journal of Diabetes & Metabolic Disorders.2022; 21(1): 181. CrossRef - Recent information on test utilization and intraindividual change in anti-glutamic acid decarboxylase antibody in Korea: a retrospective study
Rihwa Choi, Wonseo Park, Gayoung Chun, Jiwon Lee, Sang Gon Lee, Eun Hee Lee
BMJ Open Diabetes Research & Care.2022; 10(3): e002739. CrossRef - Prevalence and factors associated with latent autoimmune diabetes in adults (LADA): a cross-sectional study
Anselmo M. Manisha, Aminiel R. Shangali, Sayoki G. Mfinanga, Erasto V. Mbugi
BMC Endocrine Disorders.2022;[Epub] CrossRef - Latent Autoimmune Diabetes in Adults (LADA) and its Metabolic Characteristics among Yemeni Type 2 Diabetes Mellitus Patients
Dhekra Al-Zubairi, Molham AL-Habori, Riyadh Saif-Ali
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2021; Volume 14: 4223. CrossRef - Therapeutic approaches for latent autoimmune diabetes in adults: One size does not fit all
Theocharis Koufakis, Niki Katsiki, Pantelis Zebekakis, George Dimitriadis, Kalliopi Kotsa
Journal of Diabetes.2020; 12(2): 110. CrossRef - Long‐term effects on glycaemic control and β‐cell preservation of early intensive treatment in patients with newly diagnosed type 2 diabetes: A multicentre randomized trial
Suk Chon, Sang Youl Rhee, Kyu Jeung Ahn, Sei Hyun Baik, Yongsoo Park, Moon Suk Nam, Kwan Woo Lee, Soon Jib Yoo, Gwanpyo Koh, Dae Ho Lee, Young Seol Kim, Jeong‐Taek Woo
Diabetes, Obesity and Metabolism.2018; 20(5): 1121. CrossRef - A Global Perspective of Latent Autoimmune Diabetes in Adults
Rajashree Mishra, Kenyaita M. Hodge, Diana L. Cousminer, Richard D. Leslie, Struan F.A. Grant
Trends in Endocrinology & Metabolism.2018; 29(9): 638. CrossRef - The prevalence of latent autoimmune diabetes in adults and its correlates in patients with type 2 diabetes in Kerman, Iran [2011]
Gozashti Mohammad Hossein, Shafiei Maryam, Esmaeilian Saeed, Najafipour Hamid, Mashrouteh Mahdieh
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2015; 9(2): 104. CrossRef - Low prevalence of latent autoimmune diabetes in adults in northern India
A. Sachan, G. Zaidi, R. P. Sahu, S. Agrawal, P. G. Colman, E. Bhatia
Diabetic Medicine.2015; 32(6): 810. CrossRef - Amelioration of Diabetes-induced Cognitive Deficits by GSK-3β Inhibition is Attributed to Modulation of Neurotransmitters and Neuroinflammation
Ashok Kumar Datusalia, Shyam Sunder Sharma
Molecular Neurobiology.2014; 50(2): 390. CrossRef - Successful treatment of latent autoimmune diabetes in adults with Traditional Chinese Medicine: a case report
Jiaxing Tian, Wenke Liu, Zhong Zhen, Xiaolin Tong
Journal of Traditional Chinese Medicine.2013; 33(6): 766. CrossRef - Clinical characteristics and insulin independence of Koreans with new‐onset type 2 diabetes presenting with diabetic ketoacidosis
H. Seok, C. H. Jung, S. W. Kim, M. J. Lee, W. J. Lee, J. H. Kim, B‐W. Lee
Diabetes/Metabolism Research and Reviews.2013; 29(6): 507. CrossRef - A Case of Latent Autoimmune Diabetes in Adults Developed after Surgical Cure of Growth Hormone Secreting Pituitary Tumor
Wonjin Kim, Jung Ho Kim, Youngsook Kim, Ji Hye Huh, Su Jin Lee, Mi Sung Park, Eun Yeong Choe, Jeong Kyung Park, Myung Won Lee, Jae Won Hong, Byung Wan Lee, Eun Seok Kang, Bong Soo Cha, Eun Jig Lee, Hyun Chul Lee
Endocrinology and Metabolism.2012; 27(4): 318. CrossRef - Latent Autoimmune Diabetes in Adults: Autoimmune Diabetes in Adults with Slowly Progressive β-cell Failure
Hannah Seok, Byung Wan Lee
Diabetes & Metabolism Journal.2012; 36(2): 116. CrossRef
- The worldwide prevalence of latent autoimmune diabetes of adults among adult-onset diabetic individuals: a systematic review and meta-analysis
- Mitochondrial Dysfunction and Insulin Resistance: The Contribution of Dioxin-Like Substances
- Hong Kyu Lee
- Diabetes Metab J. 2011;35(3):207-215. Published online June 30, 2011
- DOI: https://doi.org/10.4093/dmj.2011.35.3.207
- 45,469 View
- 39 Download
- 21 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Persistent organic pollutants (POPs) are known to cause mitochondrial dysfunction and this in turn is linked to insulin resistance, a key biochemical abnormality underlying the metabolic syndrome. To establish the cause and effect relationship between exposure to POPs and the development of the metabolic syndrome, Koch's postulates were considered. Problems arising from this approach were discussed and possible solutions were suggested. In particular, the difficulty of establishing a cause and effect relationship due to the vagueness of the metabolic syndrome as a disease entity was discussed. Recently a bioassay, aryl-hydrocarbon receptor (AhR) trans-activation activity using a cell line expressing AhR-luciferase, showed that its activity is linearly related with the parameters of the metabolic syndrome in a population. This finding suggests the possible role of bioassays in the analysis of multiple pollutants of similar kinds in the pathogenesis of several closely related diseases, such as type 2 diabetes and the metabolic syndrome. Understanding the effects of POPs on mitochondrial function will be very useful in understanding the integration of various factors involved in this process, such as genes, fetal malnutrition and environmental toxins and their protectors, as mitochondria act as a unit according to the metabolic scaling law.
-
Citations
Citations to this article as recorded by- Drug-induced mitochondrial toxicity: Risks of developing glucose handling impairments
Auxiliare Kuretu, Charles Arineitwe, Mamosheledi Mothibe, Phikelelani Ngubane, Andile Khathi, Ntethelelo Sibiya
Frontiers in Endocrinology.2023;[Epub] CrossRef - Obesogens in Foods
Iva Kladnicka, Monika Bludovska, Iveta Plavinova, Ludek Muller, Dana Mullerova
Biomolecules.2022; 12(5): 680. CrossRef - Pesticides and pancreatic adenocarcinoma: A transversal epidemiological, environmental and mechanistic narrative review
Mathias Brugel, Claire Carlier, Gabriela Reyes-Castellanos, Sidonie Callon, Alice Carrier, Olivier Bouché
Digestive and Liver Disease.2022; 54(12): 1605. CrossRef - Low-Dose Dioxin Reduced Glucose Uptake in C2C12 Myocytes: The Role of Mitochondrial Oxidative Stress and Insulin-Dependent Calcium Mobilization
Suyeol Im, Sora Kang, Ji Hwan Kim, Seung Jun Oh, Youngmi Kim Pak
Antioxidants.2022; 11(11): 2109. CrossRef - Hallmarks of Health
Carlos López-Otín, Guido Kroemer
Cell.2021; 184(1): 33. CrossRef - Prenatal exposure to persistent organic pollutants and markers of obesity and cardiometabolic risk in Spanish adolescents
Nuria Güil-Oumrait, Damaskini Valvi, Raquel Garcia-Esteban, Monica Guxens, Jordi Sunyer, Maties Torrent, Maribel Casas, Martine Vrijheid
Environment International.2021; 151: 106469. CrossRef - Clinical Value of Serum Mitochondria-Inhibiting Substances in Assessing Renal Hazards: A Community-Based Prospective Study in Korea
Hoon Sung Choi, Jin Taek Kim, Hong Kyu Lee, Wook Ha Park, Youngmi Kim Pak, Sung Woo Lee
Endocrinology and Metabolism.2021; 36(6): 1298. CrossRef - Potential role of aryl hydrocarbon receptor signaling in childhood obesity
Nancy N. Shahin, Ghada T. Abd-Elwahab, Afaf A. Tawfiq, Hanan M. Abdelgawad
Biochimica et Biophysica Acta (BBA) - Molecular and Cell Biology of Lipids.2020; 1865(8): 158714. CrossRef - Potential contribution of insecticide exposure and development of obesity and type 2 diabetes
Xiao Xiao, John M. Clark, Yeonhwa Park
Food and Chemical Toxicology.2017; 105: 456. CrossRef - Persistent Organic Pollutants as Risk Factors for Obesity and Diabetes
Chunxue Yang, Alice Pik Shan Kong, Zongwei Cai, Arthur C.K. Chung
Current Diabetes Reports.2017;[Epub] CrossRef - Aryl hydrocarbon receptor deficiency protects mice from diet-induced adiposity and metabolic disorders through increased energy expenditure
C-X Xu, C Wang, Z-M Zhang, C D Jaeger, S L Krager, K M Bottum, J Liu, D-F Liao, S A Tischkau
International Journal of Obesity.2015; 39(8): 1300. CrossRef - Disruption of Ah Receptor Signaling during Mouse Development Leads to Abnormal Cardiac Structure and Function in the Adult
Vinicius S. Carreira, Yunxia Fan, Hisaka Kurita, Qin Wang, Chia-I Ko, Mindi Naticchioni, Min Jiang, Sheryl Koch, Xiang Zhang, Jacek Biesiada, Mario Medvedovic, Ying Xia, Jack Rubinstein, Alvaro Puga, Diego Fraidenraich
PLOS ONE.2015; 10(11): e0142440. CrossRef - Persistent organic pollutants and biomarkers of diabetes risk in a cohort of Great Lakes sport caught fish consumers
Mary Turyk, Giamila Fantuzzi, Victoria Persky, Sally Freels, Anissa Lambertino, Maria Pini, Davina H. Rhodes, Henry A. Anderson
Environmental Research.2015; 140: 335. CrossRef - Serum aryl hydrocarbon receptor ligand activity is associated with insulin resistance and resulting type 2 diabetes
Eun Roh, Soo Heon Kwak, Hye Seung Jung, Young Min Cho, Youngmi Kim Pak, Kyong Soo Park, Seong Yeon Kim, Hong Kyu Lee
Acta Diabetologica.2015; 52(3): 489. CrossRef - A cross-sectional analysis of dioxins and health effects in municipal and private waste incinerator workers in Japan
Kenya YAMAMOTO, Mitsuhiro KUDO, Heihachiro ARITO, Yasutaka OGAWA, Tsutomu TAKATA
INDUSTRIAL HEALTH.2015; 53(5): 465. CrossRef - Association of Dioxin and Other Persistent Organic Pollutants (POPs) with Diabetes: Epidemiological Evidence and New Mechanisms of Beta Cell Dysfunction
Vincenzo De Tata
International Journal of Molecular Sciences.2014; 15(5): 7787. CrossRef - The Glycated Albumin to Glycated Hemoglobin Ratio Might Not Be Associated with Carotid Atherosclerosis in Patients with Type 1 Diabetes
Wonjin Kim, Kwang Joon Kim, Byung-Wan Lee, Eun Seok Kang, Bong Soo Cha, Hyun Chul Lee
Diabetes & Metabolism Journal.2014; 38(6): 456. CrossRef - Pesticides and human chronic diseases: Evidences, mechanisms, and perspectives
Sara Mostafalou, Mohammad Abdollahi
Toxicology and Applied Pharmacology.2013; 268(2): 157. CrossRef - Coenzyme Q10 Ameliorates Pain and Cartilage Degradation in a Rat Model of Osteoarthritis by Regulating Nitric Oxide and Inflammatory Cytokines
Jennifer Lee, Yeon Sik Hong, Jeong Hee Jeong, Eun Ji Yang, Joo Yeon Jhun, Mi Kyoung Park, Young Ok Jung, Jun Ki Min, Ho Youn Kim, Sung Hwan Park, Mi-La Cho, Zoltan Rakonczay
PLoS ONE.2013; 8(7): e69362. CrossRef - Plasmatic concentration of organochlorine lindane acts as metabolic disruptors in HepG2 liver cell line by inducing mitochondrial disorder
Mohammed el Amine Benarbia, David Macherel, Sébastien Faure, Caroline Jacques, Ramaroson Andriantsitohaina, Yves Malthièry
Toxicology and Applied Pharmacology.2013; 272(2): 325. CrossRef - Increased Susceptibility to Metabolic Syndrome in Adult Offspring of Angiotensin Type 1 Receptor Autoantibody-Positive Rats
Suli Zhang, Xi Zhang, Lihong Yang, Zi Yan, Li Yan, Jue Tian, Xiaoyu Li, Li Song, Li Wang, Xiaoli Yang, Ronghua Zheng, Wayne Bond Lau, Xinliang Ma, Huirong Liu
Antioxidants & Redox Signaling.2012; 17(5): 733. CrossRef
- Drug-induced mitochondrial toxicity: Risks of developing glucose handling impairments
- Increasing Trend in the Number of Severe Hypoglycemia Patients in Korea
- Jin Taek Kim, Tae Jung Oh, Ye An Lee, Jun Ho Bae, Hyo Jeong Kim, Hye Seung Jung, Young Min Cho, Kyong Soo Park, Soo Lim, Hak Chul Jang, Hong Kyu Lee
- Diabetes Metab J. 2011;35(2):166-172. Published online April 30, 2011
- DOI: https://doi.org/10.4093/dmj.2011.35.2.166
- 65,535 View
- 66 Download
- 30 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background To investigate whether the number of subjects with severe hypoglycemia who are brought to a hospital emergency department is increasing and to identify whether there have been changes in the demographic and clinical characteristics of those subjects.
Methods We analyzed data from the Emergency Departments of two general hospitals in Seoul, Korea. We included data from all adult subjects with type 2 diabetes who presented to an emergency department with severe hypoglycemia between January 1, 2004 and December 30, 2009.
Results A total of 740 cases of severe hypoglycemia were identified. The mean subject age was 69±12 years, mean duration of diabetes was 13.8±9.3 years, and 53.2% of subjects were receiving insulin therapy. We observed a sharp rise in the number of cases between 2006 and 2007. Stages 3-5 chronic kidney disease was diagnosed in 31.5% of subjects, and low C-peptide levels (<0.6 ng/mL) were found in 25.5%. The mean subject age, duration of diabetes, HbA1c level, and renal and insulin secretory function values did not change significantly during the study period. The proportion of glimepiride use increased, while use of gliclazide decreased among sulfonylurea users. Use of insulin analogues increased, while use of NPH/RI decreased among insulin users.
Conclusion We identified a sharp increase in the number of subjects with severe hypoglycemia presenting to an emergency room since 2006. The clinical characteristics of these subjects did not change markedly during the study period. Nationwide studies are warranted to further clarify this epidemic of severe hypoglycemia.
-
Citations
Citations to this article as recorded by- Hypoglycemia Unawareness—A Review on Pathophysiology and Clinical Implications
Laura Hölzen, Bernd Schultes, Sebastian M. Meyhöfer, Svenja Meyhöfer
Biomedicines.2024; 12(2): 391. CrossRef - Hospital admissions trends for severe hypoglycemia in diabetes patients in Spain, 2005 to 2015
Domingo Orozco-Beltrán, Alberto Guillen-Mollá, Ana María Cebrián-Cuenca, Jorge Navarro-Pérez, Vicente F. Gil-Guillén, Jose A. Quesada, Francisco J. Pomares-Gómez, Adriana Lopez-Pineda, Concepción Carratalá-Munuera
Diabetes Research and Clinical Practice.2021; 171: 108565. CrossRef - Trends and risk factors in severe hypoglycemia among individuals with type 2 diabetes in Korea
Seung Eun Lee, Kyoung-Ah Kim, Kang Ju Son, Sun Ok Song, Kyeong Hye Park, Se Hee Park, Joo Young Nam
Diabetes Research and Clinical Practice.2021; 178: 108946. CrossRef - Predisposing factors of hypoglycemia in patients with type 2 diabetes mellitus presented with symptomatic hypoglycemia in a tertiary hospital of Bangladesh
AjitK Paul, A.B.M. Kamrul-Hasan
Journal of Diabetology.2020; 11(3): 163. CrossRef - Real-world risk of hypoglycemia-related hospitalization in Japanese patients with type 2 diabetes using SGLT2 inhibitors: a nationwide cohort study
Takeshi Horii, Yoichi Oikawa, Narumi Kunisada, Akira Shimada, Koichiro Atsuda
BMJ Open Diabetes Research & Care.2020; 8(2): e001856. CrossRef - Association between BMI and risk of severe hypoglycaemia in type 2 diabetes
J.-S. Yun, Y.-M. Park, K. Han, S.-A. Cha, Y.-B. Ahn, S.-H. Ko
Diabetes & Metabolism.2019; 45(1): 19. CrossRef - The effects of hypoglycaemia and dementia on cardiovascular events, falls and fractures and all‐cause mortality in older individuals: A retrospective cohort study
Katharina Mattishent, Kathryn Richardson, Ketan Dhatariya, George M. Savva, Chris Fox, Yoon K. Loke
Diabetes, Obesity and Metabolism.2019; 21(9): 2076. CrossRef - Detection of asymptomatic drug-induced hypoglycemia using continuous glucose monitoring in older people – Systematic review
K. Mattishent, Y.K. Loke
Journal of Diabetes and its Complications.2018; 32(8): 805. CrossRef - Incidence rate and patient characteristics of severe hypoglycemia in treated type 2 diabetes mellitus patients in Japan: Retrospective Diagnosis Procedure Combination database analysis
Yuika Ikeda, Takekazu Kubo, Eisei Oda, Machiko Abe, Shigeru Tokita
Journal of Diabetes Investigation.2018; 9(4): 925. CrossRef - A study to evaluate the prevalence of impaired awareness of hypoglycaemia in adults with type 2 diabetes in outpatient clinic in a tertiary care centre in Singapore
Ling Zhu, Li Chang Ang, Wee Boon Tan, Xiaohui Xin, Yong Mong Bee, Su-Yen Goh, Ming Ming Teh
Therapeutic Advances in Endocrinology and Metabolism.2017; 8(5): 69. CrossRef - Baseline-Corrected QT (QTc) Interval Is Associated with Prolongation of QTc during Severe Hypoglycemia in Patients with Type 2 Diabetes Mellitus
Seon-Ah Cha, Jae-Seung Yun, Tae-Seok Lim, Yoon-Goo Kang, Kang-Min Lee, Ki-Ho Song, Ki-Dong Yoo, Yong-Moon Park, Seung-Hyun Ko, Yu-Bae Ahn
Diabetes & Metabolism Journal.2016; 40(6): 463. CrossRef - Response: Cardiovascular Disease Predicts Severe Hypoglycemia in Patients with Type 2 Diabetes (Diabetes Metab J 2015;39:498-506)
Jae-Seung Yun, Yu-Bae Ahn
Diabetes & Metabolism Journal.2016; 40(1): 85. CrossRef - 1,5-Anhydro-D-Glucitol Could Reflect Hypoglycemia Risk in Patients with Type 2 Diabetes Receiving Insulin Therapy
Min Kyeong Kim, Hye Seung Jung, Soo Heon Kwak, Young Min Cho, Kyong Soo Park, Seong Yeon Kim
Endocrinology and Metabolism.2016; 31(2): 284. CrossRef - Severe Hypoglycemia and Cardiovascular or All-Cause Mortality in Patients with Type 2 Diabetes
Seon-Ah Cha, Jae-Seung Yun, Tae-Seok Lim, Seawon Hwang, Eun-Jung Yim, Ki-Ho Song, Ki-Dong Yoo, Yong-Moon Park, Yu-Bae Ahn, Seung-Hyun Ko
Diabetes & Metabolism Journal.2016; 40(3): 202. CrossRef - Hypoglycemia and Health Costs
Yong-ho Lee, Gyuri Kim, Eun Seok Kang
The Journal of Korean Diabetes.2016; 17(1): 11. CrossRef - Bi‐directional interaction between hypoglycaemia and cognitive impairment in elderly patients treated with glucose‐lowering agents: a systematic review and meta‐analysis
K. Mattishent, Y. K. Loke
Diabetes, Obesity and Metabolism.2016; 18(2): 135. CrossRef - Trend of antihyperglycaemic therapy and glycaemic control in 184,864 adults with type 1 or 2 diabetes between 2002 and 2014: Analysis of real-life data from the DPV registry from Germany and Austria
Barbara Bohn, Wolfgang Kerner, Jochen Seufert, Hans-Peter Kempe, Peter M. Jehle, Frank Best, Martin Füchtenbusch, Andreas Knauerhase, Martin Hofer, Joachim Rosenbauer, Reinhard W. Holl
Diabetes Research and Clinical Practice.2016; 115: 31. CrossRef - Characteristics of Hypoglycemia Pateints Visiting the Emergency Department of a University Hospital
Sang-Hyeon Choi, Deok-Ki Youn, Moon-Gi Choi, Ohk-Hyun Ryu
The Journal of Korean Diabetes.2016; 17(3): 202. CrossRef - Increasing trend in emergency department visits for hypoglycemia from patients with type 2 diabetes mellitus in Taiwan
Ying-Ju Chen, Chen-Chang Yang, Lynn-Chu Huang, Likwang Chen, Chii-Min Hwu
Primary Care Diabetes.2015; 9(6): 490. CrossRef - Intensive Individualized Reinforcement Education Is Important for the Prevention of Hypoglycemia in Patients with Type 2 Diabetes
Yun-Mi Yong, Kyung-Mi Shin, Kang-Min Lee, Jae-Young Cho, Sun-Hye Ko, Min-Hyang Yoon, Tae-Won Kim, Jong-Hyun Jeong, Yong-Moon Park, Seung-Hyun Ko, Yu-Bae Ahn
Diabetes & Metabolism Journal.2015; 39(2): 154. CrossRef - 1,5-Anhydroglucitol as a Useful Marker for Assessing Short-Term Glycemic Excursions in Type 1 Diabetes
Hannah Seok, Ji Hye Huh, Hyun Min Kim, Byung-Wan Lee, Eun Seok Kang, Hyun Chul Lee, Bong Soo Cha
Diabetes & Metabolism Journal.2015; 39(2): 164. CrossRef - A nationwide population-based study on the risk of coma, ketoacidosis and hypoglycemia in patients with celiac disease and type 1 diabetes
Matthew Kurien, Kaziwe Mollazadegan, David S. Sanders, Jonas F. Ludvigsson
Acta Diabetologica.2015; 52(6): 1167. CrossRef - Blood electrolyte disturbances during severe hypoglycemia in Korean patients with type 2 diabetes
Mi Yeon Kang
The Korean Journal of Internal Medicine.2015; 30(5): 648. CrossRef - Cardiovascular Disease Predicts Severe Hypoglycemia in Patients with Type 2 Diabetes
Jae-Seung Yun, Seung-Hyun Ko, Sun-Hye Ko, Ki-Ho Song, Ki-Dong Yoo, Kun-Ho Yoon, Yong-Moon Park, Yu-Bae Ahn
Diabetes & Metabolism Journal.2015; 39(6): 498. CrossRef - The Influence of Admission Hypoglycemia on Clinical Outcomes in Acute Myocardial Infarction Patients with Diabetes Mellitus
Eun Jung Kim, Myung Ho Jeong, In Seok Jeong, Sang Gi Oh, Sang Hyung Kim, Young keun Ahn, Ju Han Kim, Young Jo Kim, Shung Chull Chae, Taek Jong Hong, In Whan Seong, Jei Keon Chae, Chong Jin Kim, Myeong Chan Cho, Ki Bae Seung, Hyo Soo Kim
Korean Journal of Medicine.2014; 87(5): 565. CrossRef - Corrected QT Interval Prolongation during Severe Hypoglycemia without Hypokalemia in Patients with Type 2 Diabetes
Jae Won Beom, Jung Min Kim, Eun Joo Chung, Ju Yeong Kim, Seung Yeong Ko, Sang Don Na, Cheol Hwan Kim, Gun Park, Mi Yeon Kang
Diabetes & Metabolism Journal.2013; 37(3): 190. CrossRef - Presence of Macroalbuminuria Predicts Severe Hypoglycemia in Patients With Type 2 Diabetes
Jae-Seung Yun, Sun-Hye Ko, Sun-Hee Ko, Ki-Ho Song, Yu-Bae Ahn, Kun-Ho Yoon, Yong-Moon Park, Seung-Hyun Ko
Diabetes Care.2013; 36(5): 1283. CrossRef - Severe Hypoglycemia in Patients with Diabetes
Jae Seung Yun, Seung-Hyun Ko
Diabetes & Metabolism Journal.2012; 36(4): 273. CrossRef - Severe hypoglycaemia requiring the assistance of emergency medical services - frequency, causes and symptoms
Veronika Krnacova, Ales Kubena, Karel Macek, Martin Bezdek, Alena Smahelova, Jiri Vlcek
Biomedical Papers.2012; 156(3): 271. CrossRef - Higher Morning to Evening Ratio in Total Dose of Twice-Daily Biphasic Insulin Analog Might Be Effective in Achieving Glucose Control in Patients with Poorly Controlled Type 2 Diabetes
Yong-Ho Lee, Byung-Wan Lee, Hea Jin Kwon, Eun Seok Kang, Bong Soo Cha, Hyun Chul Lee
Diabetes Technology & Therapeutics.2012; 14(6): 508. CrossRef
- Hypoglycemia Unawareness—A Review on Pathophysiology and Clinical Implications
- Polymorphisms of the
Reg 1α Gene and Early Onset Type 2 Diabetes in the Korean Population - Bo Kyung Koo, Young Min Cho, Kuchan Kimm, Jong-Young Lee, Bermseok Oh, Byung Lae Park, Hyun Sub Cheong, Hyoung Doo Shin, Kyung Soo Ko, Sang Gyu Park, Hong Kyu Lee, Kyong Soo Park
- Korean Diabetes J. 2010;34(4):229-236. Published online August 31, 2010
- DOI: https://doi.org/10.4093/kdj.2010.34.4.229
- 3,532 View
- 23 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background The
Reg gene has been reported to be expressed in regenerating islets and Reg1 protein to be up-regulated at an early stage of diabetes in mice. As humanReg 1α is homologous with murineReg 1, we investigated whether common variants inReg 1α are associated with type 2 diabetes in the Korean population.Methods We sequenced the
Reg 1α gene to identify common polymorphisms using 24 Korean DNA samples. Of 11 polymorphisms found, five common ones (g.-385T>C [rs10165462], g.-36T>G [rs25689789], g.209G>T [rs2070707], g.1385C>G [novel], and g.2199G>A [novel]) were genotyped in 752 type 2 diabetic patients and 642 non-diabetic subjects.Results No polymorphism was associated with the risk of type 2 diabetes. However, g.-385C and g.2199A lowered the risk of early-onset type 2 diabetes, defined as a diagnosis in subjects whose age at diagnosis was 25 years or more but less than 40 years (odds ratio [OR], 0.721 [0.535 to 0.971] and 0.731 [0.546 to 0.977] for g.-385C and g.2199A, respectively) and g.1385G increased the risk of early-onset diabetes (OR, 1.398 [1.055 to 1.854]). Although adjusting for errors in multiple hypotheses-testing showed no statistically significant association between the three individual polymorphisms and early-onset diabetes, the haplotype
H1 , composed of g.-385C, g.1385C, and g.2199A, was associated with a reduced risk of early-onset diabetes (OR, 0.590 [0.396 to 0.877],P = 0.009).Conclusion Polymorphisms in the
Reg 1α were not found to be associated with overall susceptibility to type 2 diabetes, though some showed modest associations with early-onset type 2 diabetes in the Korean population.-
Citations
Citations to this article as recorded by- Glycemic Effects of Once-a-Day Rapid-Acting Insulin Analogue Addition on a Basal Insulin Analogue in Korean Subjects with Poorly Controlled Type 2 Diabetes Mellitus
Eun Yeong Choe, Yong-ho Lee, Byung-Wan Lee, Eun-Seok Kang, Bong Soo Cha, Hyun Chul Lee
Diabetes & Metabolism Journal.2012; 36(3): 230. CrossRef
- Glycemic Effects of Once-a-Day Rapid-Acting Insulin Analogue Addition on a Basal Insulin Analogue in Korean Subjects with Poorly Controlled Type 2 Diabetes Mellitus
- Effect of Adipose Differentiation-Related Protein (ADRP) on Glucose Uptake of Skeletal Muscle.
- Yun Hyi Ku, Min Kim, Sena Kim, Ho Seon Park, Han Jong Kim, In Kyu Lee, Dong Hoon Shin, Sung Soo Chung, Sang Gyu Park, Young Min Cho, Hong Kyu Lee, Kyong Soo Park
- Korean Diabetes J. 2009;33(3):206-214. Published online June 1, 2009
- DOI: https://doi.org/10.4093/kdj.2009.33.3.206
- 2,141 View
- 24 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Skeletal muscle is the most important tissue contributing to insulin resistance. Several studies have shown that accumulation of intramyocellular lipid is associated with the development of insulin resistance. Thus, proteins involved in lipid transport, storage and metabolism might also be involved in insulin action in skeletal muscle. Adipose differentiation-related protein (ADRP), which is localized at the surface of lipid droplets, is known to be regulated by peroxisome proliferator activated receptor gamma (PPARgamma). However, it is not known whether ADRP plays a role in regulating glucose uptake and insulin action in skeletal muscle. METHODS: ADRP expression in skeletal muscle was measured by RT-PCR and western blot in db/db mice with and without PPARgamma agonist. The effect of PPARgamma agonist or high lipid concentration (0.4% intralipos) on ADRP expression was also obtained in cultured human skeletal muscle cells. Glucose uptake was measured when ADRP was down-regulated with siRNA or when ADRP was overexpressed with adenovirus. RESULTS: ADRP expression increased in the skeletal muscle of db/db mice in comparison with normal controls and tended to increase with the treatment of PPARgamma agonist. In cultured human skeletal muscle cells, the treatment of PPARgamma agonist or high lipid concentration increased ADRP expression. siADRP treatment decreased both basal and insulin-stimulated glucose uptake whereas ADRP overexpression increased glucose uptake in cultured human skeletal muscle cells. CONCLUSION: ADRP expression in skeletal muscle is increased by PPARgamma agonist or exposure to high lipid concentration. In these conditions, increased ADRP contributed to increase glucose uptake. These results suggest that insulin-sensitizing effects of PPARgamma are at least partially achieved by the increase of ADRP expression, and ADRP has a protective effect against intramyocellular lipid-induced insulin resistance.
- Prevalence and Clinical Characteristics of Aspirin Resistance in the Patients with Type 2 Diabetes Mellitus.
- Mi Yeon Kang, Young Min Cho, Hyun Kyung Kim, Jee Hyun An, Hwa Young Ahn, Ji Won Yoon, Hoon Sung Choi, Jie Seon Lee, Kyong Soo Park, Seong Yeon Kim, Hong Kyu Lee
- Korean Diabetes J. 2008;32(1):53-59. Published online February 1, 2008
- DOI: https://doi.org/10.4093/kdj.2008.32.1.53
- 2,490 View
- 22 Download
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
We examined the prevalence and clinical characteristics of aspirin resistance in the Korean patients with type 2 diabetes mellitus. METHODS: We studied 181 Korean patients with type 2 diabetes mellitus who were taking aspirin (100 mg/day for > or = 3 months) and no other antiplatelet agents. The VerifyNow System was used to determine aspirin responsiveness. Aspirin resistance was defined as an aspirin reaction unit (ARU) > or = 550. We measured the cardio-ankle vascular index (CAVI) and ankle-brachial index (ABI) to evaluate arteriosclerosis. The anthropometric parameters, electrocardiogram, blood pressure, fasting plasma glucose, lipid profiles, hemoglobin A1c, highly sensitive C-reactive protein (hsCRP), homocysteine, and microalbuminuria were measured in each patient. RESULTS: The prevalence of aspirin resistance in type 2 diabetic patients was 9.4% (17 of 181). Those who had aspirin resistance were older than those without aspirin resistance (64.6 +/- 10.6 vs. 59.8 +/- 8.1, P = 0.024). Aspirin resistance was not associated with fasting plasma glucose, total cholesterol, triglyceride, LDL-cholesterol, HDL-cholesterol, hemoglobin A1c, hsCRP, homocysteine, microalbuminuria, ABI, CAVI, and body mass index. CONCLUSION: Prevalence of aspirin resistance in the Korean patients with type 2 diabetes mellitus was 9.4%. Although aspirin resistance was associated with old age, we could not find any good clinical parameter to predict it. Therefore, aspirin resistance should be evaluated in diabetic patients taking aspirin for prevention of cardiovascular complications. -
Citations
Citations to this article as recorded by- Long Non-Coding RNA H19 Positively Associates With Aspirin Resistance in the Patients of Cerebral Ischemic Stroke
Jue Wang, Bin Cao, Yan Gao, Dong Han, Haiping Zhao, Yuhua Chen, Yumin Luo, Juan Feng, Yanxia Guo
Frontiers in Pharmacology.2020;[Epub] CrossRef - 6th Asian PAD Workshop
Annals of Vascular Diseases.2015; 8(2): 135. CrossRef - Non-HDL cholesterol is an independent risk factor for aspirin resistance in obese patients with type 2 diabetes
Jong Dai Kim, Cheol-Young Park, Kue Jeong Ahn, Jae Hyoung Cho, Kyung Mook Choi, Jun Goo Kang, Jae Hyeon Kim, Ki Young Lee, Byung Wan Lee, Ji Oh Mok, Min Kyong Moon, Joong Yeol Park, Sung Woo Park
Atherosclerosis.2014; 234(1): 146. CrossRef
- Long Non-Coding RNA H19 Positively Associates With Aspirin Resistance in the Patients of Cerebral Ischemic Stroke
- Two Cases of Autoantibody Negative Fulminant Type 1 Diabetes Mellitus.
- Hwa Young Cho, Young Min Cho, Myoung Hee Park, Mi Yeon Kang, Ki Hwan Kim, Yun Hyi Ku, Eun Kyung Lee, Do Joon Park, Chan Soo Shin, Kyong Soo Park, Seong Yeon Kim, Bo Youn Cho, Hong Kyu Lee
- Korean Diabetes J. 2007;31(4):372-376. Published online July 1, 2007
- DOI: https://doi.org/10.4093/jkda.2007.31.4.372
- 2,211 View
- 16 Download
-
 Abstract
Abstract
 PDF
PDF - Autoantibody negative fulminant type 1 diabetes mellitus is a novel subtype of type 1 diabetes, which is characterized by a remarkably abrupt onset, metabolic derangement such as diabetic ketoacidosis at diagnosis, low HbA1c level at onset and a negative islet-related autoantibodies. The prevalence of fulminant type 1 diabetes has large difference between Japan and other countries. The precise reason for this regional variation remains to be clarified. One of the possible explanations is genetic background such as genotype of class II HLA molecule. In addition, environment factors including viral infection are suggested as possible pathogenesis of the disease. Only a few cases with fulminant type 1 diabetes have been reported outside Japan, and most of these cases with definite diagnosis have been reported in Korea. We report here on two Korean patients that met the criteria for diagnosis of fulminant type 1 diabetes in accordance with their HLA genotypes.
- The Association of Aldose Reductase Gene Polymorphisms with Neuropathy in Patients with Type 2 Diabetes.
- In Kyong Jeong, Kyong Soo Park, Min Kyong Moon, Jae Hyeon Kim, Chan Soo Shin, Seong Yeon Kim, Hong Kyu Lee
- Korean Diabetes J. 2007;31(3):274-283. Published online May 1, 2007
- DOI: https://doi.org/10.4093/jkda.2007.31.3.274
- 1,914 View
- 17 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Previous studies have suggested that polymorphisms in and around the aldose reductase (AR) gene are associated with the development of diabetic microvascular disease. This study explored the hypothesis that the polymorphisms of the (A-C)n dinucleotide repeat sequence, located at 2.1 kilobase (kb) upstream of the transcription start site of AR gene, modulate the risk of diabetic neuropathy (DN). METHODS: 66 patients with DN, 30 without microvascular complications (MC) after 20 years of diabetes, and 87 normal healthy controls were studied. To test highly polymorphic microsatellite marker 2.1 kb upstream of the initiation site of the AR gene, we performed polymerase chain reaction using the primer labeled with fluorescent dye and GeneScan by ABI prism 377 automated DNA sequencer and ABI Genotyper software 2.0. RESULTS: Seven alleles (Z-6, Z-4, Z-2, Z, Z+2, Z+4 and Z+6) were identified. Z-2 allele was more frequently observed in patients with DN (77.3%) than in those without MC (43.3%, P = 0.007). The subgroup of patients who developed DN within 5 years after the diagnosis of diabetes also had higher frequency of Z-2 allele (91.7%) compared to those without MC (43.3%, P = 0.028). On the contrary, Z+6 allele tended to be more frequent in patients without MC (10.0%) than in those with DN (0%, P = 0.063). CONCLUSION: These results support the hypothesis that environmental-genetic interactions may modulate the risk of neuropathy in patients with diabetes. Particularly, the Z-2 allele, in the presence of diabetes, may be associated with the development of DN. -
Citations
Citations to this article as recorded by- The Association between Serum GGT Concentration and Diabetic Peripheral Polyneuropathy in Type 2 Diabetic Patients
Ho Chan Cho
Korean Diabetes Journal.2010; 34(2): 111. CrossRef
- The Association between Serum GGT Concentration and Diabetic Peripheral Polyneuropathy in Type 2 Diabetic Patients
- Retraction: Polymorphisms of Kir6.2 Gene are Associated with Type 2 Diabetes and Blood Pressure in the Korean Population.
- Bo Kyeong Koo, Hong Il Kim, Eu Jin Lee, Young Min Cho, Hyoung Doo Shin, Hak Chul Jang, Hong Kyu Lee, Kyong Soo Park
- Korean Diabetes J. 2007;31(2):185-185. Published online March 1, 2007
- DOI: https://doi.org/10.4093/jkda.2007.31.2.185
- 1,674 View
- 19 Download
- Polymorphisms of Kir6.2 Gene are Associated with Type 2 Diabetes and Blood Pressure in the Korean Population.
- Bo Kyeong Koo, Hong Il Kim, Eu Jin Lee, Young Min Cho, Hyoung Doo Shin, Hak Chul Jang, Hong Kyu Lee, Kyong Soo Park
- Korean Diabetes J. 2005;29(5):440-450. Published online September 1, 2005
- 1,023 View
- 18 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGOUND: ATP-sensitive potassium channels are a heterooctamer of SUR1 and Kir6.2, which are key components in the insulin secretory mechanism. Whether common variants in the Kir6.2 gene are associated with type 2 diabetes and/or its associated phenotypes was investigated. METHODS: The Kir6.2 gene was sequenced in 24Korean DNA samples to identify common polymorphisms (frequency > 0.05). The common variants found among these samples were genotyped in a larger population including type 2 diabetic patients and nondiabetic subjects. RESULTS: Thirteen single nucleotide polymorphisms and one insertion/deletion polymorphism were identified in the Kir6.2 gene, with six common variants(g.-1709A>T, g.-1525T>C, g.67G >A [E23K], g.570C>T [A190A], g.1009A>G [1337V], and g.1388C>T) genotyped in 761 type 2 diabetic patients and 675 nondiabetic subjects. Four individual polymorphisms(g.-1525T > C, g.67G>A, g.1009A>G and g.1388C>T) appeared to be associated with type 2 diabetes (age, sex and BMI-adjusted odds ratio[OR]=0.751[0.584-0.967] in the recessive model on g-1525T>C, 1.193 [1.020-1.394] in the additive model in g.67G>A, 1.195 [1.022-1.399] in the additive model on g.1009A>G, 0.835 [0.717-0.973] in the additive model in g.1388C >T). The haplotype "ATACGC" in the Kir6.2 gene, composed of rare allele in the g.67 and g.1009, was also associated with a higher prevalence of type 2 diabetes (age, sex, and BMI- adjusted OR = 1.256 [1.067-1.479], P for logistic regression = 0.006). In addition g.67G>A and g.1009A >G in the KCNJ11 were strongly associated with a high systolic blood pressure. CONCLUSION: Polymorphisms in the Kir6.2 gene are associated with type 2 diabetes and blood pressure in the Korean population.
- Increasing Trends of Metabolic Syndrome in Korea -Based on Korean National Health and Nutrition Examination Surveys-.
- Soo Lim, Eun Jung Lee, Bo Kyeong Koo, Sung Il Cho, Kyong Soo Park, Hak Chul Jang, Seong Yeon Kim, Hong Kyu Lee
- Korean Diabetes J. 2005;29(5):432-439. Published online September 1, 2005
- 1,374 View
- 25 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGOUND: The number of individuals with metabolic syndrome is increasing in Asian as well as in Western countries. The aim of this study was to compare the prevalence and patterns of metabolic syndrome as determined by the 1998 and 2001 Korean National Health and Nutrition Examination Surveys(KNHANES). METHODS: A total of 6,907 and 4,536 Koreans aged over 20 years participated in the KNHANES in 1998 and 2001, respectively. A stratified multistage probability sampling design and weighting adjustments were made to obtain a representative Korean population. The working definition of the National Cholesterol Education Program-Adult Treatment Panel III was used to define metabolic syndrome. The International Obesity Task Force criteria for the Asian-Pacific population were used to determine waist circumference criteria. RESULTS: The age-adjusted prevalence of metabolic syndrome significantly increased from 22.5 to 24.1% between 1998 and 2001(P<0.01). Of the five components composing metabolic syndrome, low HDL-cholesterolemia showed the highest increase(32.6%) over this period, followed by hypertriglyceridemia and abdominal obesity, with 15.9% and 4.3% increases, respectively. In contrast, the number of subjects with high blood pressure or elevated fasting glucose levels were reduced(37.1-->33.1% and 18.9-->15.4%, respectively, both P<0.01). CONCLUSION: Dyslipidemia and abdominal obesity were primarily responsible for the increase in metabolic syndrome in Korea over the period 1998 to 2001. Changes to diet patterns and a reduction in physical activity are likely to have contributed to the rapid increase in metabolic syndrome in Korea; therefore, national strategies will be needed to counteract this increase.

 KDA
KDA
 First
First Prev
Prev





